Tuesday, December 20, 2011
Short Dental Implants? Is the tide turning?
Sunday, December 11, 2011
Small Mirrors ?
I've been trying to get these sizes locally for some time without success. Can anyone who is reading this help
?
Friday, December 9, 2011
Sinus floor elevation using osteotome technique without grafting materials: a 2-year retrospective study
Abstract
Objective
The study aimed to assess the clinical results after osteotome technique to lift sinus floor, without graft materials in the residual bone height (RBH), below 8 mm.
Material and methods
Twenty-two patients aged from 19 to 70 years old in need of maxillary sinus floor augmentation were enrolled in this study. Preoperative and postoperative cone beam computerized tomography (CBCT) were taken to guide the surgery. Twenty-seven implants were inserted and followed clinically, another CBCT exam was taken at 6 months postoperatively. The diameter of the implants was 4.7 mm (SD 0.4 mm), the length was 10 mm (SD 1.0 mm). The average residual bone height was 6.7 mm (SD 1.2 mm).
Results
No implants were lost after the surgery and the 2 years follow-up. There was no obvious marginal bone loss during the 6 months follow-up verified by CBCT. The mean bone gain at the implant sites was 2.5 mm (SD 1.5 mm).
Conclusion
The study verified the good and stable clinical result of the OSFE technique without using bone grafting materials when the RBH was only 4.1–8 mm.
Wednesday, December 7, 2011
Implant Survival Rates after Osteotome-Mediated Maxillary Sinus Augmentation: A Systematic Review
ABSTRACT
Purpose: The aim of the present study was to systematically evaluate the implant survival rate after osteotome-mediated maxillary sinus augmentation with or without using grafting materials.
Materials and Methods: MEDLINE database was searched using a combination of specific search terms. Furthermore, a hand searching of the relevant journals and of the bibliographies of reviews was performed. Prospective and retrospective clinical studies with at least 20 patients treated by osteotome-mediated sinus floor elevation were included.
Results: Nineteen studies were selected for data analysis. A total of 1,822 patients, accounting for 3,131 implants were considered. Mean weighted cumulative implant survival at 1, 2, 3, and 5 years was estimated as 98.12%, 97.40%, 96.75%, and 95.81%, respectively. No significant difference was found in relation to the use of grafting material nor in relation to implant length. Overall implant survival was 92.7% for 331 implants placed in <5 mm ridge height and 96.9% for 2,525 implants inserted in ≥5 mm ridge height. The difference was significant (p = .0003).
Conclusions: The transalveolar sinus augmentation technique could be a viable treatment in case of localized atrophy in the posterior maxilla even in case of minimal residual bone height. The prognosis can be more favorable when the residual ridge is at least 5 mm high.
Sunday, October 16, 2011
InQu Bone Graft Extender/Substitute Receive CE Mark Approval

Bone grafting is one of the cornerstones of orthopaedic surgery. In cases like trauma, tumors, fusions and skeletal reconstruction there are often spaces and gaps that need to be filled in with bone. This is where bone grafting comes into play, and there are many options. The best bet is to use bone harvested from the patient, such as iliac crest bone graft from the pelvis. This is termed autograft and contains bone-producing stem-cells, growth factors and a structural scaffold to provide mechanical stability. In cases where a surgeon would like to avoid the pain and risk associated with harvesting bone, there are less invasive options. You can use bone obtained from organ donors, termed allograft (also less appropriately dubbed “croutons”). Allograft, however, carries the risk of infection and other transplant associated problems. Then there are bone graft substitutes/extenders, synthetic bioactive materials that provide a scaffold for healing bone to grow into. These usually are the least effective, however they can be combined with various modalities such as bone marrow aspirate to be a safe and effective (although more expensive) alternative to traditional bone grafting.
So in related news, ISTO just announced that their InQu Bone Graft extender/substitute material just received CE Mark approval (it received 510(k) clearance in the US in 2007). The product is somewhat unique, in that it combines polylactide-co-glycolide (PLGA) and unmodified hyaluronicacid (HyA), which are materials not commonly found in most commercially available bone graft substitutes. There is little research available regarding the effectiveness of this combination in skeletal surgery in the extremities, but it sounds promising. The PLGA is meant to provide an osteoconductive scaffold while the HyA improves handling, cell attachment and supports vascular ingrowth. It is designed for use in non-structural areas of bone, such as small voids from benign tumor excisions or hardware removals. The material is available as granules, a paste, putty and 3-dimensional structures.
Wednesday, September 21, 2011
How To Do High-Quality 3D Bone Model Printing On The Cheap
 Orthopedic and maxillofacial surgeons sometimes prepare for surgery by creating physical models of 3D scans of bones that they need to work on. Such models are also useful in educating med school students, doctors, and patients. However, these models tend to be very expensive, usually seen only in well-funded research projects or used by expensive medical professionals. Oftentimes, because the cost of the model is so high, a compromise must be made, so the resulting models end up being truncated or less than actual size.
Orthopedic and maxillofacial surgeons sometimes prepare for surgery by creating physical models of 3D scans of bones that they need to work on. Such models are also useful in educating med school students, doctors, and patients. However, these models tend to be very expensive, usually seen only in well-funded research projects or used by expensive medical professionals. Oftentimes, because the cost of the model is so high, a compromise must be made, so the resulting models end up being truncated or less than actual size.
Shapeways, a company that prints custom-designed 3D models, published a blog post about how Max Frame, an orthopedic surgeon at the Royal Hospital for Sick Children in Glasgow, Scotland, managed to produce a full-size human pelvis for about $230, less than one-fifth the cost of a smaller, professionally made model.

He accomplished this by taking CT scans and importing them into two programs, one to fill in any gaps and eliminate any artifacts on the CT scan and the other to create a 3D surface render that Shapeways can read. After being sent to Shapeways, it took less than a week for Max to receive the models. According to Max, the models were verified and shown to be virtually identical to the bones in the CT scan. Moreover, the white plastic that composed the models proved to be a great bone analog in which to practice using regular orthopedic drills, screws, and saws.
Blog entry from Shapeways: 3D Printing Bone on a budget!
Thursday, September 15, 2011
Medtronic launches Artisan System for Bone Graft Protection In Oral-Maxillofacial Surgery
 Bone grafting is the use of either native, cadaveric, or artifical bone pieces to fill a void where you would like new bone to grow. Often at first, bone grafts have poor structural qualities and need hardware to protect them, the bone around and to keep them in place. In Oral-Maxillofacial surgery bone loss is often caused by infection, trauma, tumors and other conditions.
Bone grafting is the use of either native, cadaveric, or artifical bone pieces to fill a void where you would like new bone to grow. Often at first, bone grafts have poor structural qualities and need hardware to protect them, the bone around and to keep them in place. In Oral-Maxillofacial surgery bone loss is often caused by infection, trauma, tumors and other conditions.
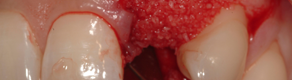
Medtronic has announced the launch of its Artisan space maintenance system which is a set of a customizable titanium mesh, special screws for mesh fixation, as well as socket screws. The mesh is specifically designed for the protection of bone graft and has unique handling and structural properties for this purpose. The socket screws in particular are being marketed as ground breaking since the umbrella-shaped screw design allows for the protection of bone graft while eliminating the need to lift a second flap for the removal of the screw.
Press release: Medtronic Announces Launch of ARTISAN™ Space Maintenance System
Thursday, August 25, 2011
A Cavity-Filling Fluid That Regenerates Tooth Enamel – Is This The End Of The Dental Drill?
 Perhaps someday, the bi-annual trip to the dentist may become much less intimidating, thanks to researchers at Leeds University in the UK who have developed a completely pain-free way to fill cavities.
Perhaps someday, the bi-annual trip to the dentist may become much less intimidating, thanks to researchers at Leeds University in the UK who have developed a completely pain-free way to fill cavities.
Taking inspiration from the principles of regenerative medicine, the process involves a special peptide-based fluid. Suspended in water, the peptide fluid, known as P 11-4 is clear and has a similar viscosity as water. Under certain conditions, namely when placed in contact with saliva that surrounds a tooth, the fluid forms a gel scaffold that fills the microscopic holes that are cavities. The scaffold, which mimics proteins that are found in growing teeth, attracts hydroxyapatite and other minerals to regenerate actual tooth enamel within weeks.
If P 11-4 is shown to be effective in larger clinical trials, the feared dental drill may one day find its place on the shelf with other archaic, barbaric medical devices from our past!
Here’s a video report about the research from UK’s Channel 4:
Article from Leeds University: Filling Without Drilling…
Wednesday, August 24, 2011
Bioactive Compound Can Be Molded to Fit Grafting Site
 NovaBone Products has introduced a new line of biologically active bone-graft substitutes that are designed to enhance the body’s natural healing process by facilitating rapid vascularization and mineralization. Suspended in a rapidly-absorbable binder, the moldable material contains a calcium phosphosilicate with a continuous macroporous structure. Known as MacroPor-Si+, the product can be used to repair osseous defects throughout the skeletal system.
NovaBone Products has introduced a new line of biologically active bone-graft substitutes that are designed to enhance the body’s natural healing process by facilitating rapid vascularization and mineralization. Suspended in a rapidly-absorbable binder, the moldable material contains a calcium phosphosilicate with a continuous macroporous structure. Known as MacroPor-Si+, the product can be used to repair osseous defects throughout the skeletal system.
Founded in 2002, the manufacturer offers a variety of silicon- and calcium-ion controlled-release products that stimulate the regeneration of cortical and cancellous bone.
Press release: NovaBone Announces New Moldable Bone Graft…
Manufacturer’s web site: NovaBone Products…
Saturday, July 2, 2011
Updates to Dropbox Terms of Service and Privacy Statement
| |||
| |||
 © 2011 Dropbox © 2011 Dropbox |
Tuesday, April 19, 2011
Economies of small
Economies of scale are well understood. Bigger factories are more efficient, bigger distribution networks are more efficient, bigger ad campaigns can be more efficient. It's often hard to defeat a major competitor, particularly if the market is looking for security and the status quo.
But what about the economies of small? Is being bigger an intrinsic benefit in and of itself?
If your goal is to make a profit, it's entirely possible that less overhead and a more focused product line will increase it.
If your goal is to make more art, it's entirely possible the ridding yourself of obligations and scale will help you do that.
If your goal is to have more fun, it's certainly likely that avoiding the high stakes of more debt, more financing and more stuff will help with that.
I think we embraced scale as a goal when the economies of that scale were so obvious that we didn't even need to mention them. Now that it's so much easier to produce a product in the small and market a product in the small, and now that it's so beneficial to offer a service to just a few, with focus and attention, perhaps we need to rethink the very goal of scale.
Don't be small because you can't figure out how to get big. Consider being small because it might be better.
Thursday, April 7, 2011
I Can't Shut My Mouth and All I Can Do Is Scream
Here's a cute story of a girl who yawned so hard in class that her jaw misaligned. A bit of clinical trickery using wood tongue depressors and a steady hand of the doctor is what's in the prescription. The responsible party is, of course, the professor for not being lively enough for this student.
From BBC Three Bizarre ER show:
(hat tip: Gizmodo)
Monday, March 21, 2011
Interpositional osteotomies for the atrophic posterior mandible - A Concept whose time has come?
| ||
Implant Rehabilitation of the Edentulous Posterior Atrophic Mandible: The Sandwich Osteotomy Revisited Jose Luis López-Cedrún, MD, DDS, PhD | ||
Purpose: Treatment of the posterior atrophic mandible has long been a challenge in implant dentistry and maxillofacial surgery. The objective of this study was to reevaluate the safety and efficacy of the sandwich osteotomy and bone grafting in patients with moderate to severe posterior mandibular atrophy. Materials and Methods: This retrospective study included patients with an edentulous posterior mandible in which there was not enough bone above the dental nerve to insert implants at least 10 mm in length; patients with adequate bone volume but with an excessive interocclusal distance at the posterior occlusal region were also included. Twenty-three patients with 30 sites of moderate to severe posterior atrophy were treated using a sandwich osteotomy above the mental nerve and an interpositioned block of autologous or allogeneic bone. Success criteria were based on the possibility of implant insertion after bone grafting. Results: The average gain in height was 5.3 mm (range, 2 to 10 mm). Partial loss of alveolar height was observed in only one patient from the allogeneic graft group. Patients were followed for 12 to 93 months after bone grafting. No signs of infection were observed. Minor dehiscence of the surgical wound occurred in four segments, but healing ultimately occurred in every patient. Sixty-five implants were placed, and none were lost during follow-up. Insertion of implants of 10 mm or more in length was successfully achieved in 90.8% of the sites, and partial success (ie, bone segments suitable for insertion of shorter implants) was seen in the remaining sites. Conclusions: Moderate to severe posterior mandibular atrophy can be successfully treated by interpositional sandwich osteotomy and bone grafting, allowing for the subsequent placement of implants and fixed prostheses in all segments. Int J Oral Maxillofac Implants 2011;26:195–202 Key words: atrophic mandible, dental implants, inlay bone grafting, sandwich osteotomy |
Sunday, March 20, 2011
Does Elevating The Sinus Membrane Without Bone Grafting Really Work?
| ||
New Bone Formation Following Sinus Membrane Elevation Without Bone Grafting: Histologic Findings in Humans Jae-Jin Ahn, DDS, MS, PhD/Sung-Am Cho, DDS, MS, PhD/Gerard Byrne, DDS/Jae-Hyun Kim, DDS, MS/Hong-In Shin, DDS, PhD | ||
Purpose: To determine whether sinus membrane elevation alone can lead to new bone formation on the maxillary sinus floor. Materials and Methods: Among patients who were to receive implant treatment, those who had 4 to 5 mm of bone height in the maxillary sinus floor (as measured radiographically) were selected as candidates for sinus membrane elevation. The lateral sinus wall was exposed through a buccal mucoperiosteal incision. The sinus membrane was elevated through a bone window, and the space underneath the membrane was filled with absorbable collagen sponge (Collaplug). In the presence of blood in the space, the collagen sponge was left to soak up the blood; in the deficiency of blood, the sponge was saturated with venous blood drawn from the brachial vein. The mucoperiosteal flap was repositioned and closed with interrupted silk sutures. The sinus was left to heal for 6 months. Core specimens of the maxillary sinus floor were obtained using a trephine bur at 6 months after sinus elevation in patients treated between January 2006 and June 2009. The trephined sites were used for implant placement. The biopsy specimens were analyzed histologically to identify the presence and amount of new bone tissue. Results: Thirteen specimens from eight patients were included in the study. Microscopically, 11 specimens exhibited no recognizable new bone tissue. Two specimens exhibited a small amount of woven bone on the surface of the sinus floor. Conclusion: Within the limits of this study of eight patients, little to no new bone formation was observed on the maxillary sinus floor at 6 months following sinus membrane elevation and support with blood-soaked collagen sponges. Int J Oral Maxillofac Implants 2011;26:83–90 Key words: bone formation, bone graft, lateral window, maxillary sinus, membrane elevation, sinus floor augmentation |
Friday, March 18, 2011
Low Risk of Jaw Problems With Oral Osteoporosis Drugs
Wednesday, March 9, 2011
Fwd: This Month in Compendium of Continuing Education in Dentistry
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

--
Dr.C.P.Mathai MDS
Oral Surgery, Dental Implants, Oral Reconstruction.
Restoring Smiles! Building Confidence!
http://www.implantsutra.com