| ||
Implant Rehabilitation of the Edentulous Posterior Atrophic Mandible: The Sandwich Osteotomy Revisited Jose Luis López-Cedrún, MD, DDS, PhD | ||
Purpose: Treatment of the posterior atrophic mandible has long been a challenge in implant dentistry and maxillofacial surgery. The objective of this study was to reevaluate the safety and efficacy of the sandwich osteotomy and bone grafting in patients with moderate to severe posterior mandibular atrophy. Materials and Methods: This retrospective study included patients with an edentulous posterior mandible in which there was not enough bone above the dental nerve to insert implants at least 10 mm in length; patients with adequate bone volume but with an excessive interocclusal distance at the posterior occlusal region were also included. Twenty-three patients with 30 sites of moderate to severe posterior atrophy were treated using a sandwich osteotomy above the mental nerve and an interpositioned block of autologous or allogeneic bone. Success criteria were based on the possibility of implant insertion after bone grafting. Results: The average gain in height was 5.3 mm (range, 2 to 10 mm). Partial loss of alveolar height was observed in only one patient from the allogeneic graft group. Patients were followed for 12 to 93 months after bone grafting. No signs of infection were observed. Minor dehiscence of the surgical wound occurred in four segments, but healing ultimately occurred in every patient. Sixty-five implants were placed, and none were lost during follow-up. Insertion of implants of 10 mm or more in length was successfully achieved in 90.8% of the sites, and partial success (ie, bone segments suitable for insertion of shorter implants) was seen in the remaining sites. Conclusions: Moderate to severe posterior mandibular atrophy can be successfully treated by interpositional sandwich osteotomy and bone grafting, allowing for the subsequent placement of implants and fixed prostheses in all segments. Int J Oral Maxillofac Implants 2011;26:195–202 Key words: atrophic mandible, dental implants, inlay bone grafting, sandwich osteotomy |
Monday, March 21, 2011
Interpositional osteotomies for the atrophic posterior mandible - A Concept whose time has come?
Sunday, March 20, 2011
Does Elevating The Sinus Membrane Without Bone Grafting Really Work?
| ||
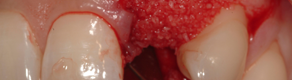
New Bone Formation Following Sinus Membrane Elevation Without Bone Grafting: Histologic Findings in Humans Jae-Jin Ahn, DDS, MS, PhD/Sung-Am Cho, DDS, MS, PhD/Gerard Byrne, DDS/Jae-Hyun Kim, DDS, MS/Hong-In Shin, DDS, PhD | ||
Purpose: To determine whether sinus membrane elevation alone can lead to new bone formation on the maxillary sinus floor. Materials and Methods: Among patients who were to receive implant treatment, those who had 4 to 5 mm of bone height in the maxillary sinus floor (as measured radiographically) were selected as candidates for sinus membrane elevation. The lateral sinus wall was exposed through a buccal mucoperiosteal incision. The sinus membrane was elevated through a bone window, and the space underneath the membrane was filled with absorbable collagen sponge (Collaplug). In the presence of blood in the space, the collagen sponge was left to soak up the blood; in the deficiency of blood, the sponge was saturated with venous blood drawn from the brachial vein. The mucoperiosteal flap was repositioned and closed with interrupted silk sutures. The sinus was left to heal for 6 months. Core specimens of the maxillary sinus floor were obtained using a trephine bur at 6 months after sinus elevation in patients treated between January 2006 and June 2009. The trephined sites were used for implant placement. The biopsy specimens were analyzed histologically to identify the presence and amount of new bone tissue. Results: Thirteen specimens from eight patients were included in the study. Microscopically, 11 specimens exhibited no recognizable new bone tissue. Two specimens exhibited a small amount of woven bone on the surface of the sinus floor. Conclusion: Within the limits of this study of eight patients, little to no new bone formation was observed on the maxillary sinus floor at 6 months following sinus membrane elevation and support with blood-soaked collagen sponges. Int J Oral Maxillofac Implants 2011;26:83–90 Key words: bone formation, bone graft, lateral window, maxillary sinus, membrane elevation, sinus floor augmentation |
Friday, March 18, 2011
Low Risk of Jaw Problems With Oral Osteoporosis Drugs
Wednesday, March 9, 2011
Fwd: This Month in Compendium of Continuing Education in Dentistry
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

--
Dr.C.P.Mathai MDS
Oral Surgery, Dental Implants, Oral Reconstruction.
Restoring Smiles! Building Confidence!
http://www.implantsutra.com